Understanding the Postpartum Period
The postpartum period, often called the "fourth trimester," begins immediately after childbirth and lasts about six weeks. During this time, your body experiences significant changes as it recovers from pregnancy and birth.
Physically, you can expect:
- uterine contractions as your uterus returns to its pre-pregnancy size
- vaginal bleeding (lochia) that gradually decreases
- tenderness in the perineal area or near any incisions or repairs
- breast changes, including engorgement as your milk comes in
- general discomfort
Emotionally, it's normal to experience:
- mood swings, often called the "baby blues"
- feelings of being overwhelmed or anxious
- tiredness or exhaustion from lack of sleep
- adjustments to new routines and responsibilities
Common Postpartum Complications
- physical changes the body goes through
- underlying health conditions
- the birthing process itself
- what signs to look out for and
- when to seek help.
Postpartum Hemorrhage
Risk factors include:
- prolonged labor
- multiple pregnancies
- large baby
- previous PPH
Signs and symptoms:
- soaking more than one sanitary pad per hour
- large blood clots (the size of an egg or larger)
- drop in blood pressure, causing dizziness or fainting
- rapid heartbeat
Infections and Sepsis
Potential signs of infection to watch for include:
- fever over 100.4°F (38°C)
- severe abdominal pain
- foul-smelling vaginal discharge
- redness, swelling, or discharge from incision sites
- breast pain, redness, or flu-like symptoms (mastitis)
To prevent infections:
- practice good hygiene, especially hand washing
- keep incision sites clean and dry
- empty your bladder and change sanitary pads regularly
- wear breathable, cotton underwear
- complete full courses of prescribed antibiotics
- attend all postpartum check-ups
What is Sepsis?
Sepsis warning signs to watch for:
- fever over 100.4°F (38°C)
- chills and sweats
- rapid heart rate
- rapid breathing
- extreme pain or discomfort
- confusion or disorientation
- clammy or sweaty skin
Postpartum Preeclampsia
Symptoms include:
- severe headaches
- changes in vision, like blurriness or seeing spots
- upper abdominal pain
- swelling in the face or hands
- high blood pressure
Blood Clots
Risk factors include:
- cesarean delivery
- obesity
- prolonged bed rest
- personal or family history of blood clots
Symptoms to watch for:
- swelling in one leg or arm
- pain or tenderness in the affected area
- skin that is warm to the touch, hard, red, or discolored
- chest pain and difficulty breathing if the clot travels to the lungs (pulmonary embolism)
To reduce your risk:
- move around frequently, even if you're on bed rest
- stay hydrated
- wear compression stockings if recommended by your doctor
- avoid crossing your legs, sitting, or lying down for long periods (except while sleeping).
Mental Health Issues
Symptoms include:
- persistent sadness or emptiness
- loss of interest in activities you used to enjoy
- difficulty bonding with your baby
- changes in sleep or appetite
- thoughts of harming yourself or your baby
Breast-related Complications
- Engorgement: When milk comes in, your breasts may become overly full, hard, and painful. Nursing or pumping frequently to meet the baby's nutritional needs (without over-pumping) can help your body regulate milk supply and keep you more comfortable until engorgement subsides.
- Blocked ducts: These can cause a painful lump in the breast. To prevent overstimulation of the affected breast, offer the breast without the plug first. Avoid deep massage. After expressing, lightly sweep the breast tissue (like petting a cat) from the nipple toward the armpit and collarbone. Apply cold compresses after feeding to relieve pain and swelling.
- Mastitis: This painful breast infection causes flu-like symptoms and a red, tender area on the breast. It requires prompt treatment with antibiotics.
To prevent breast complications:
- Ensure proper latch and positioning during breastfeeding.
- Nurse or pump regularly to meet your baby's nutritional needs. However, wait until your milk supply is well-established before pumping and storing extra milk for future use.
- Wear a supportive, well-fitting bra.
Pelvic Floor Disorders
Symptoms of pelvic floor disorders include:
- leaking urine when coughing, sneezing, or exercising
- difficulty controlling bowel movements
- a feeling of heaviness or pressure in the vagina
When to Seek Medical Help
Resources for New Parents
- Your healthcare provider is there to help and guide you. Please don't hesitate to contact them with questions about your health. They can direct you to resources available in your community.
- Postpartum Support International (www.postpartum.net)
- La Leche League for breastfeeding support (www.llli.org)
- Join a local new parent support group. These can often be found by contacting your local hospital or community center.
- Connect with an online support community: search your preferred social media channel and join a few support groups that match your interest.
- Trusted online resources like the American College of Obstetricians and Gynecologists (www.acog.org) or the American Academy of Pediatrics (healthychildren.org).
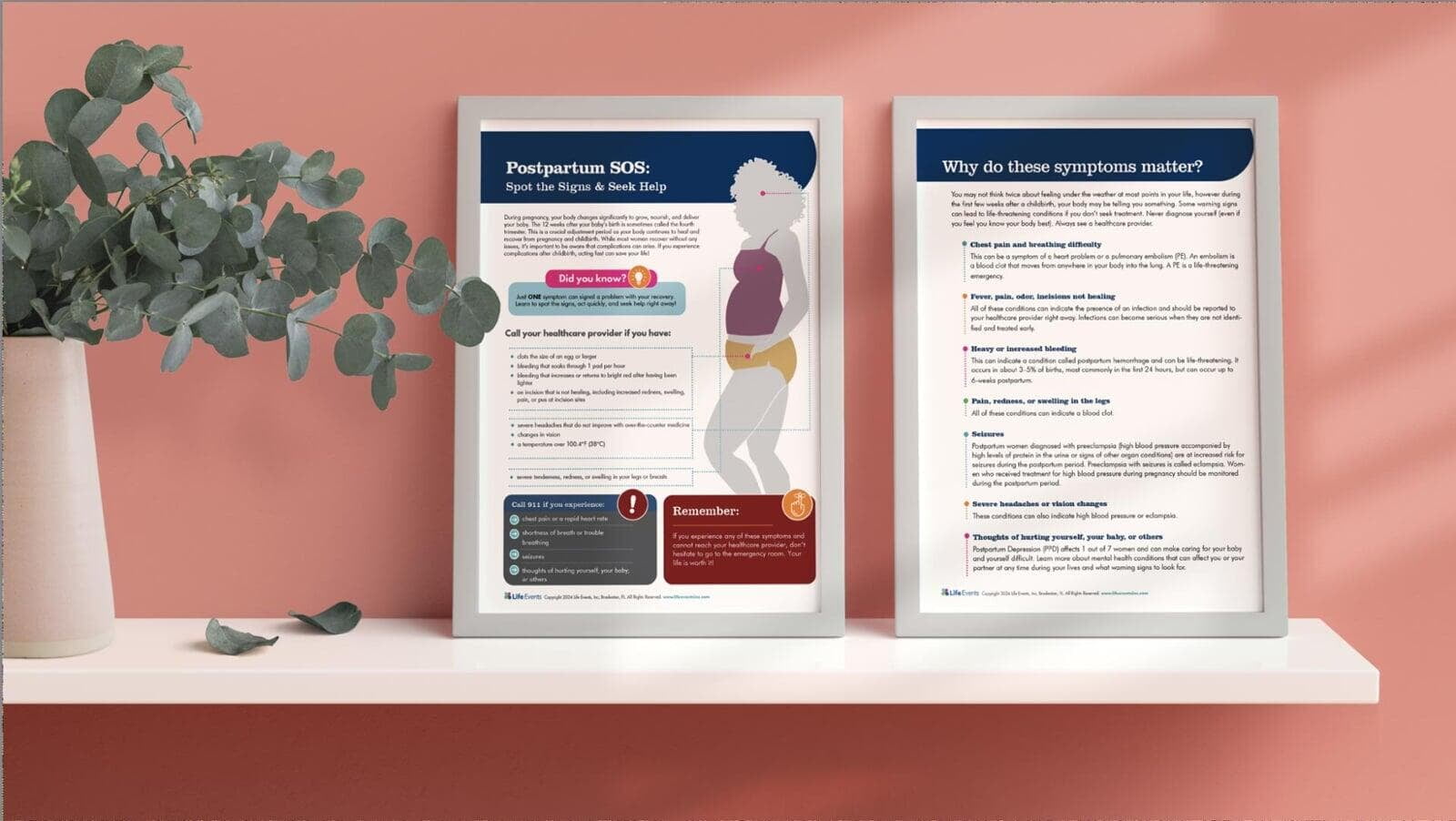
Identify Postpartum Complications Early with Our SOS Flyer
Our easy-to-read Postpartum SOS: Spot the Signs and Seek Help flyer helps you recognize potential complications early on. Whether you're a healthcare professional sharing this vital resource or a new parent taking charge of your health, this flyer is an essential, life-saving tool. Access with a code or find it on our Etsy shop.
Final Thoughts
Final Thoughts
#PostpartumComplications #PostpartumRecovery #FourthTrimester #MomLife #PelvicFloorHealth #PostpartumHemorrhage #KnowThePostpartumWarningSigns #RecoveryAfterDelivery #LifeEventsInc
Sources
Baby News: Caring for Yourself and Your Newborn. Life Events, Inc., Bradenton, FL, 2024.
Preparing for Labor and Childbirth. Life Events, Inc., Bradenton, FL, 2024.